The adoption of new medical technologies - a focus on outcomes and value
Medical devices – is value-based healthcare a help or a hindrance?
Any innovative intervention in healthcare should demand us
to ask of ourselves the problem we are
trying to solve, the desired outcome for
this individual, and the associated
costs and ramifications for the wider healthcare system. Nowhere is this more
true than in the development and adoption of diagnostic, monitoring and
therapeutic medical devices.
An evidence-based path to adoption of novel devices which
may be of very high value to patients has been problematic, as highlighted by
the recent excellent article by Campbell et al, ‘Generating evidence for new
high-risk medical devices’. Additionally there are differences between the
type of data collection required and evidence needed to support HTA decision
making between diagnostic and therapeutic devices.
What we are seeking to do is achieve value for patients (in
terms of the outcomes that matter to them) and healthcare providers and
governments who are under pressure to balance resource allocation to meet
multiple needs of patients across the population they serve.
Therefore we want to adopt novel devices quickly when they
show a lot of promise but also subsequently ensure that they deliver on that
promise in the lives of real people. We can and should back up that decision
making with ongoing outcome data capture including patient-reported outcomes as
part of real world evidence generation. The push towards value-based healthcare
is helpful in this regard as it encourages the embedding of patient-reported
outcome data capture into direct care, thereby making it a more sustainable
endeavour with the ability to create more robust data sets. The implementation
of patient-reported outcome measurement should never be set up as a data
collection exercise alone. Patient -reported outcomes can enhance the
communication between patients and their clinical teams and therefore have a
range of uses in supporting shared decision making, acting as triggers for key
conversations and as a needs assessment, long before we have acquired larger
datasets for value analysis.
Much has already been said about the need for a new
relationship between industry and healthcare systems, particularly in considering
new contracting models based on patient outcomes. This should not be
misunderstood, as this new relationship with industry is not about driving the
medical industrial complex in isolation without taking account of the impact of
an intervention on the whole system of care for patients. We accept that
industry has to be profitable. However, to achieve maximum value for patients
we need to also ensure that we undertake two additional activities.
The first of these is of course to minimise unnecessary costs
by adopting the most cost effective product on the market. Careful attention to
outcomes is necessary in order to make this judgment.
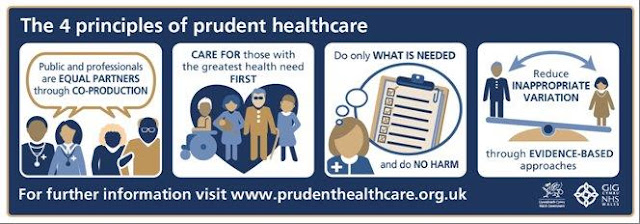
The second is to ensure optimal positioning of devices in
the patient pathway. Does evidence based medicine not achieve this? If we look
at any atlas of variation on device utilisation it would appear not. For
example, the use of implantable devices for patients with advanced heart
failure often correlates only with the proximity of the patient’s home to the tertiary
centre. Unwarranted variation, both over- and under-treatment exist and we must
tackle both. If we look at the definition of evidence-based medicine as
outlined by David Sackett, we may be able to guess at the answer why.
• ‘Evidence-based
practice is the conscientious, explicit and judicious use of current best
evidence in making decisions about the care of the individual patient. It means
integrating individual clinical expertise with the best available external
clinical evidence from systematic research.’
• ‘The
patient brings to the encounter his or her own personal preferences and unique
concerns, expectations, and values.’
Crucially, evidence-based guidelines tend to miss out the
second part about the patient’s context and the shared understanding of their
situation with their clinician. This in turn may subsequently influence choices
made about the appropriateness of an intervention for that individual including
whether to receive a medical device. This problem impacts on monitoring devices,
for example CGM in diabetes or telemetry in heart failure; and therapeutic
devices, for example implantable defibrillators or resynchronisation devices in
heart failure patients.
Condition-specific patent-reported outcome data are
essentially structured communications about symptoms and health status between
an individual and their clinician. It therefore provides information both about
need and about impact of an intervention on quality of life in a very specific
way. Unlike generic measures of quality of life such as the EQ5D, it is
generally harder to generate QALYs (quality adjusted life years), the
comparable measure of cost effectiveness usually employed by health economists
as part of the bases for a health technology assessment. However, I would argue
that these measures give us much more information about the impact of an
intervention.
If we can embed patient-reported outcome measures as a
useful activity in the direct care of patients, and find ways to use this data
including in the generation of QALYs from condition-specific tools, then we
will enhance our ability to assess the value of medical devices and their true
impact on the lives of patients.

Comments
Post a Comment