Navigating the Covid seas - time to focus on what really matters
Recovering from Covid-19 – maintaining a focus on
outcomes
The
Covid-19 pandemic has generated an extraordinary response from the healthcare
system in transforming the way that we work in order that we operate in a way
that minimises spread of infection and allows services to cope during a surge
of cases of viral infection. However, this came at a price with the temporary
cessation of virtually all outpatient and elective activity in hospitals. We
have in our response moved to remote triage for all patients in primary care
and have seen a rapid rise in the use of video consulting to support safe
decision making. Face to face consultations have been minimised and QOF
activity has been formally postponed.
Change has
happened at great speed and been made possible through a considerable cutting
of red tape, using the goodwill and flexibility of the workforce and digitally
supported remote management. Some of this system change in healthcare delivery
is positive and should be captured and adopted for the longer term benefit of
everyone. We have a duty to ensure that services essential for people with
non-Covid time-sensitive problems are able to function so that outcomes are not
adversely affected by the necessary pandemic response. The WHO has issued guidance
on this topic:
The importance of this is heightened as we
know that it is likely that society will be living with this pandemic until a
vaccination is available. For this reason continued vigilance and flexibility
are needed to be able to step up the specific responses to the virus as
necessary.
This is a
highly complex and uncertain scenario which requires decisions to be made
within an ethical framework in order that we balance the competing risks to
achieve the best outcomes for the whole population. A focus on equity is
needed; equity in geographical provision of services and also between patient
groups with differing needs. Particular attention is required to work against inequities
caused by social deprivation and ethnicity which may grow during the pandemic, as
well as vulnerable groups such as those with learning disabilities, care home
residents or those needing palliative care.
There will
be competing demands from different specialties on supporting services such as
radiology, pathology and theatres as colleagues begin to tackle the backlog of
people waiting for treatment. Undoubtedly there will be a need for
prioritisation of those in greatest need to be brought to the front of the
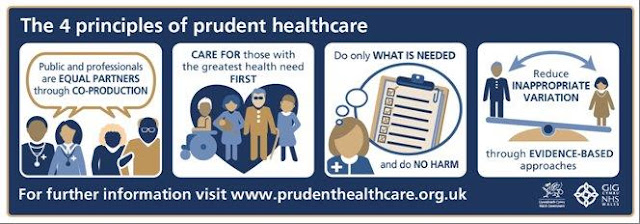
queue. This makes we think of one of my old blogs on this site on the second principle of Prudent
Healthcare:
'Care for those with the greatest health need first'
'Care for those with the greatest health need first'
It won’t
be easy at all as we put the wheels back on the wagon, still with the threat of
Covid-19 hanging over us, the will to deliver against a plethora of gold
standard single disease guidelines and the ongoing need to avoid
healthcare-transmitted viral infection.A focus on outcomes across the board is
therefore essential for maintaining equitable healthcare during the pandemic.
Lockdown
is not benign, neither is the virus. We must ensure that essential services for
life threatening, life changing or time sensitive conditions are maintained and
that outcomes for those with non-Covid illness do not suffer. The only way to
know this, and to avoid otherwise invisible harm, is to track outcomes. Referral
to treatment time is not a useful metric in isolation.
We must
use all tools available to us to safely meet the needs of greater numbers of
people in ways that does not always require a physical visit to a healthcare
facility. Remote management is necessary to protect patients from exposure to
infection during the pandemic but is also arguably often less of a burden in
terms of travel for those who prefer it. Telephone and video consultations do
not increase capacity in the system as they take up clinician time, but
‘asynchronous’ communication can be a tremendous aid to sustainability. Patient-reported outcomes
allow structured communication, enabling triage and informing flexible and
patient-led access to their clinical teams.
Of
particular note so far has been the growth in enthusiasm for rolling out
patient-facing technology. That has really helped us to take a leap forward
with the digital communication necessary for us to capture PROMs at scale and
in a way that is meaningful and useful for patients.
Because of
the need to manage more vulnerable groups remotely there has also been a
renewed interest in how we tackle issues of digital exclusion. Large numbers of people were ‘shielded’ and have to be managed remotely. PROMs offers a structured
assessment to support safe remote management as part of a package of care. They
will also be critical in how we manage the back log of patients waiting for
treatment in the post-Covid recovery phase to help us prioritise safely and
meet the greatest need first.
In many
ways the pandemic has created the perfect storm for the NHS and we will not have
the luxury of returning to how things were if we are to treat all our patients,
and equitably maintain outcomes. It is more important than ever to focus on
value for all patients and so the Post-Covid
recovery phase should be characterised by a process of stop, resume and reset:
Stop - there are undoubtedly some low value practices (from everybody’s perspective) that we should stop for good. I am thinking about unnecessary imaging, procedures of limited evidence and appointments which leave patients wondering why they made the trip.
Stop - there are undoubtedly some low value practices (from everybody’s perspective) that we should stop for good. I am thinking about unnecessary imaging, procedures of limited evidence and appointments which leave patients wondering why they made the trip.
Resume - there are
things that we need to resume quickly to maintain good outcomes. this can't be a bunfight of the specialities. We must work collectively if we are to ensure the best outcomes, prioritising the time-sensitive issues.
Reset - and there
are things that we should reset,
capitalising on learning from the pandemic to deliver higher value care for our
patients in the future in ways that are sustainable and meet our needs in the 21st century.
This blog will shortly be published as an editorial in the Journal of General and Family Medicine

Comments
Post a Comment