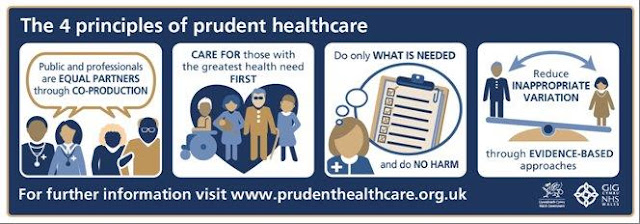
The Prudent Healthcare Blogs - Variety is not the spice
Principle four - Reduce inappropriate variation through evidence-based approaches

Unwarranted variation is a term coined by Dr John Wennberg, founder of the Centre for Evaluative Clinical Services at Dartmouth Medical School in the United States. He defined it as variation in healthcare delivery that cannot be explained by illness, medical need or evidence.
The idea that we should identify and reduce variation in healthcare is decades old and has been worked on by such giants of modern healthcare as Don Berwick and Muir Gray.
So what is it, why should we tackle it and what does that mean for clinicians and the people they care for?
Variation types:
1. Variation in the delivery of care we know to be effective and safe
For example, patients with atrial fibrillation receiving anticoagulation to prevent stroke or adherence to surgical checklists to reduce errors and improve safety, underuse of retinopathy screening for people with diabetes, and so on.
2. Preference-sensitive care. This refers to care where there are often trade offs between the benefits and risks of the intervention. Therefore in order to achieve the best outcomes, the quality of shared decision making must be high, the individual being assisted by their clinician in navigating the current evidence base and arriving at the best choice for their context. Examples could be knee replacement surgery or treatment choices in early prostate cancer. The aim here is to remove as much clinician bias as possible.
3. Supply sensitive care. This tends to be professionally or system driven care and can result in an overuse of healthcare that is not beneficial to patients. A really good example of this is seen in outpatient follow ups where historically the system has a tendency to sequentially follow people up at arbitrary intervals irrespective of whether they are currently well or in urgent need.
Sometimes this also refers to the ongoing practice of an intervention which new evidence has now shown to be less effective than previously thought.
Evidence-based medicine is defined as 'the conscientious, explicit, and judicious use of current best evidence in making decisions about the care of individual patients'. (Sackett) We know that medical practice is notoriously slow to adapt to new knowledge, particularly in abandoning outmoded interventions now found to be of limited benefit.
The reasons why we need to tackle unwarranted variation should now be clear - it can lead to harm and it definitely leads to waste, so we must do our best to reduce it if we are to create a sustainable healthcare system and hence its appearance in Prudent Healthcare, Realistic Medicine, Carter Report, GIRFT and so on.
But we need to be careful. Our information is often incomplete and in some areas variation data often raises more questions than it immediately answers. When we are looking at referral and prescribing data from primary care for example, there may be external reasons for variation, such as lack of alternatives on offer. This has certainly been the case in mental health as we have seen huge growth in antidepressant prescribing linked to lack of availability of talking therapies. We simply do not yet have the means to reliably capture variation due to patient preference, or to understand to what extent clinician behaviour is influenced by requests from patients to refer, test or prescribe. We need to understand real world patient outcomes much better and seek to reduce unwarranted variation in those outcomes, making sure that we are making true comparisons. The GIRFT programme may go some way towards this over time.
We still need to tackle variation but we need to do it sensitively and with great care. Variation which may compromise patient safety should be our priority and should be set apart from other types of variation, requiring greater scrutiny.
Most of all we must look at the system through the eyes of a person needing care. Supporting people to make good choices to meet their health goals and giving them the ability to lead their own care and maintain as much independence as possible will help us deliver the right care at the right time.
Comments
Post a Comment