The impact of incentivisation on general medical practice
In late 2003 I was a
junior partner in a primary care medical practice serving roughly 8000 patients
on the south coast of England. General practice had been going through the
doldrums, pay was low, morale was low and there was dissatisfaction with the
contract with the NHS. (Looking back, the problems pale into insignificance
compared with the current situation in UK general practice).The Labour
government of the day sought to change that through radical changes to the GP
contract with far reaching implications including the removal of 24 hour
responsibility for one’s own patients and the introduction of a
performance-related element to the remuneration of practices.
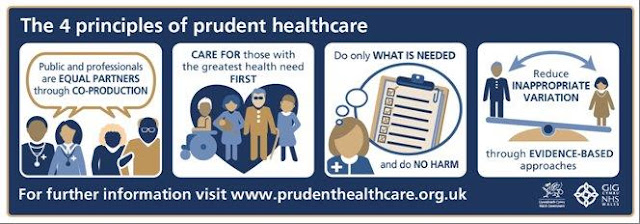
This latter element was the QoF – the Quality and Outcomes
Framework for general practice- which rewarded practices for carrying out a
series of process indicators with the aim of reducing unwarranted variation in
chronic disease management, business and clinical governance, education and
training of staff. On the one hand this was a good thing and could be seen as
evidence-based medicine driving up standards. On the other, this came with the
assumption that strict adherence to processes always produces a good outcome
for the individual patient and will improve population outcomes as a whole. Interestingly,
emerging data from the last fifteen years show that QoF actually had little if
any impact on clinical outcomes over that time and may even have caused some
harm. We can speculate why this may be so and look at the effect that
incentivisation has on medical care.
Prior to the introduction of the new contract most practices
were still using the old paper-based Lloyd George notes system and mine was no
exception. Moving to the new contract meant a rapid shift to electronic records
and the introduction of performance-related measures meant that everything had
to be codified. As the most junior partner in the practice, it fell to me to
oversee the process of summarising and coding all of the patient records,
creating the disease registers and setting up the call and recall systems for
systematic chronic disease management. It was a mammoth task but has given us
incredible insight into the nature and prevalence of disease in our practice
populations. Of course, reliable and standard coding of processes was also
essential for payment and I recall one of my colleagues being questioned by the
local Primary Care Organisation about the prevalence of type 2 diabetes in her
practice because it was higher than that predicted. These were the first
indicators we had of dynamic trends in chronic disease.
I remember having mixed feelings. There is no doubt that QoF
had beneficial effects in making us far more proactive about chronic disease
management, including chasing those who didn’t attend. But it had other unintended
consequences too…practice began to feel less than holistic, targets were not
always tailored to individual needs and preferences and there was a massive increase in target-driven
workload of questionable value that had a negative impact on access to
appointments. Many GPs felt that they were looking at the screen, not the patient,
and patients will tell you that they knew when they were being ‘qof’d’!
What then, is the impact of incentivisation? Analysis of
retired QoF indicators shows a reduction in the rate of coding of these
indicators. Does this represent a deterioration in quality of care? Perhaps,
but it is not that straightforward. Consider the recording of smoking status in
adults and the documentation that retinopathy screening has taken place. Both
of these things are outside of the control of the GP. Now let’s consider the
annual testing of cholesterol and cholesterol control in the secondary prevention
of stroke and coronary heart disease. Does this make any difference when the
patient is already on maximum dose of lipid-lowering medication? Arguably not
and arguably wasteful. More worryingly perhaps, there has been a reduction in
the recording of body mass index and glycosylated haemoglobin in people living
with serious mental illness. This could indicate a fall in proactive preventive
care in this high risk and vulnerable group, particularly as the focus shifts
towards rapid universal access. The NHS is a like a pie with only so much to go
around and a target in one area inevitably leads to a reduction in focus
somewhere else.
Advocates for the QoF approach would argue that when QoF was
felt to be inappropriate for individual patients we were free to ‘exception
report’ from the register. However, in practice, exception reporting was
frequently discouraged by Primary Care Organisations and practices faced
financial and reputational risks if they failed to score highly. The pressure
to comply was high.
If you pay people to carry out and code a process they will
do it, particularly in a high compliance environment. When the incentive is
removed, the first thing to go is the coding and associated administrative
tasks which are now defunct. This isn’t necessarily linked to outcomes because
you are paying for the code , not the activity which still may continue
unlabelled.
Financial incentives will always be a good way of nudging
organisations towards what is perceived to be good practice but we must always
be mindful of the possible unintended consequences of such incentives. At best
QoF decreased unwarranted variation in bundles of care processes. At worst it
created both over-and under-medicalisation, disutility of care and even harm
through inappropriately aggressive pursuit of clinical targets. If we think of
outcomes as milestones or endpoints that really matter to patients then we have
a long way to go if we are to measure and incentivise that happening. I remain
optimistic.

Comments
Post a Comment