Shared understanding before decision making
Whilst messing about on social media this weekend I stumbled
across some conversations that gave me a bit of a jolt. Shared decision making,
that pillar of the consultation in healthcare, something I thought was an
unassailable pursuit, was under attack. Some even commented that it should be
ditched altogether. In favour of what I thought? A return to paternalism? Perish
the thought! I was incensed! I couldn’t stop thinking about this and wondering
why some of my medical colleagues around the world had turned against this
approach and were now describing it in a number of disparaging ways. Views
ranged from it being a rather pompous term where the rhetoric far outstrips the
reality to being something which is an assault on patient autonomy or in some
cases, an assault on physician autonomy. In some cases, surely, doctor knows
best?
Shared decision making has been described as ‘a process in
which both the patient and the physician contribute to the decision-making
process.’ Other related terms have been coined such as ‘no decision about me,
without me’.
I found myself nodding in agreement that good shared
decision making tends to be aspirational rather than a consistent reality. Some
of us try harder than others, but in spite of all our efforts we are really not
as good at involving people in decisions about their healthcare as we think we
are.
I wanted to think a little more deeply about why it is so
difficult, but first to tackle something with which I am not in agreement, and
that is the notion that shared decision making is somehow a bad thing and
should be ditched.
Using the Beauchamp and Childress’ old ethical framework as
a guide let’s look at the issue of autonomy.
Patient autonomy means that an individual must be able to make their own
decisions about their health without undue influence. It is the basis for
informed consent and also means that people can make what the practitioner may
regard as being unwise choices. It is entirely up to the individual. However,
this does not absolve the doctor of the duty to inform sensitively and
factually about the likely outcomes of different courses of action.
What about decisions made autonomously by the physician? These days this refers to the doctor making the decisions on behalf of the patient based on today’s
evidence-based guidelines. There are a few emergency situations where this is
entirely appropriate and sensible but in most cases is and should be seen as
paternalistic at best. No decision about me without me. However, some people may request that the practitioner makes a decision on their behalf. This carries even greater responsibility to explore the beliefs and wishes of the individual seeking help.
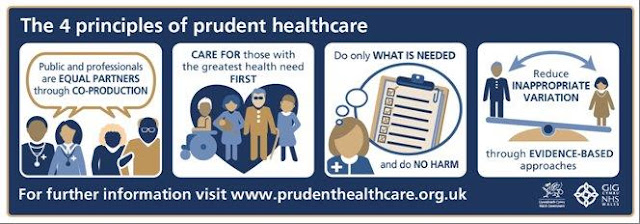
The ethical principle of autonomy does not exist in
isolation but must be considered in line with the other principles of
beneficence (promote what is good and in the best interests of the patient),
non-maleficence (do no harm) and justice (fairness, equity and respect for
rights and law). To achieve the best
outcome, both sides must share the knowledge that they have. The patient shares
their context, wishes and goals whilst the physician shares their medical
knowledge. Marrying the two sides together, we arrive at a course of action
bespoke for that individual’s circumstances.
That is the ideal scenario and the reality is often far from
this ideal. There are blind spots and knowledge gaps on both sides and usually a serious lack of time. The advice
we give as medical practitioners is riddled with ‘pseudo-certainty’ and we
often exercise our own clinical biases (often unconsciously) either over – or
under-playing the benefits and risks of this or that intervention. Surely then
in an ever more complex medical world shared decision making is more important
for us to master than ever. Together we can work towards what I think is better
described as the ‘shared understanding of medicine’ (courtesy of Professor
Richard Lehman) . Otherwise we reduce medicine to a merely technical discipline
of algorithms, orders and procedures which will neither help our patients nor
nourish us as individuals.

Comments
Post a Comment